At Hoima Regional Referral Hospital in Western Uganda, Tulinawe Kabaami anxiously watches over her 3-year-old son, who has been severely ill with malaria for five days. Tulinawe recalls how her son’s condition worsened after they first sought treatment at a local health center. “He became very weak one evening, so I gave him medication, but he didn’t improve. The next day, he collapsed and became unconscious. We rushed him to the hospital, but they had to refer us here because his condition was so serious,” she explained.
Even though the government provided the family with mosquito nets, Tulinawe admits they haven’t been using them. So far, the family has spent about $100 on medical treatment, but her son’s health has shown little improvement. To afford the costs, they had to sell some of their belongings. The rising cost of malaria treatment is a heavy burden, especially now that donors have told the government to fund the fight against malaria on their own.
Dr. Gilbert Ategeka, a pediatrician at the hospital, has observed a concerning trend—three out of every ten children admitted test positive for malaria. He highlighted the issue of improper use of mosquito nets, noting, “People use the nets for fishing instead of sleeping under them to prevent malaria. The government needs to educate families about the economic and health impacts of malaria. If a child falls ill, parents have to spend money on hospital bills, and children miss school. Village health teams (VHTs) should be encouraged and supported to teach people how to properly use mosquito nets.”
While global efforts have invested $3.5 billion in malaria prevention, more than twice that amount is needed to achieve the goal of eliminating malaria by 2030. African governments, already struggling with weak healthcare systems and limited resources, face a serious funding gap, which could have devastating consequences.
At a recent meeting alongside the World Health Organization’s Regional Committee for Africa in Brazzaville, the RBM Partnership expressed deep concern about the rise in malaria cases and deaths, particularly in Africa, where 90% of cases occur. Dr. Michael Adekunle Charles, CEO of the RBM Partnership, called this an “unacceptable injustice,” noting that malaria disproportionately affects vulnerable populations already suffering from poverty, conflict, and other inequalities.
Dr. Charles emphasized the importance of a multi-sectoral approach, saying, “Malaria intersects with other social and economic issues. When combined with poverty, rising conflicts, displacement, climate change, and gender inequalities, it creates an even bigger injustice. We must address these challenges together.”
The fight against malaria is becoming increasingly difficult, as both the malaria parasite and the mosquitoes that carry it are evolving to resist treatment and insecticides. Dr. Charles stressed the urgency of outpacing these biological threats, warning, “We must act fast to outsmart malaria before it outsmarts us. The fact that most of the world eliminated malaria decades ago while Africa continues to struggle with it is a clear sign that we are not doing enough.”
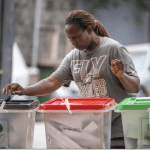
Eleven African countries—Burkina Faso, Cameroon, the Democratic Republic of Congo, Ghana, Mali, Mozambique, Niger, Nigeria, Sudan, Uganda, and Tanzania—account for 70% of global malaria deaths. These countries, which also rank low on the Human Development Index, signed the Yaoundé Declaration in March, committing to reduce malaria deaths and take more serious steps to eliminate the disease.
Although the UN Sustainable Development Goals (SDGs) set an ambitious target to end malaria by 2030, only $3.5 billion has been invested toward that goal. This falls far short of the $7.3 billion needed to eradicate malaria. African governments, already grappling with weak health systems and economic challenges, are facing a $1.5 billion funding shortfall, which threatens their ability to maintain even basic malaria prevention measures.
If funding does not increase to meet the growing needs, the RBM Partnership warns that the shortfall could result in a surge in malaria deaths, repeating the worst-case scenarios predicted at the onset of the COVID-19 pandemic.